The Sacroiliac Joint
Sacroiliac joint
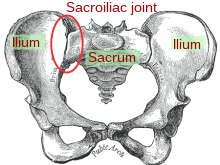
The sacroiliac joint or SI joint is the joint in the bony pelvis between the sacrum and the ilium of the pelvis, which are joined together by strong ligaments. In humans, the sacrum supports the spine and is supported in turn by an ilium on each side. The joint is a strong, weight bearing synovial joint with irregular elevations and depressions that produce interlocking of the two bones.[1] The human body has two sacroiliac joints, one on the left and one on the right, that often match each other but are highly variable from person to person.[1]
Contents
|
Anatomy
The sacroiliac joints are two paired “kidney bean” or L-shaped joints having a small amount of movement (2–18 degrees, which is debatable at this time) that are formed between the articular surfaces of the sacrum and the ilium bones.[2][3][4][5][6][7] The two sacroiliac joints move together as a single unit and are considered bicondylar joints (where the two joint surfaces move correlatively together).[8] The joints are covered by two different kinds of cartilage; the sacral surface has hyaline cartilage and the ilial surface has fibrocartilage.[9] The SIJ’s stability is maintained mainly through a combination of only some bony structure and very strong intrinsic and extrinsic ligaments.[10] As we age the characteristics of the sacroiliac joint change.[11] The joint’s surfaces are flat or planar in early life but as we start walking, the sacroiliac joint surfaces develop distinct angular orientations (and lose their planar or flat topography.) They also develop an elevated ridge along the ilial surface and a depression along the sacral surface.[12] ridge and corresponding depression, along with the very strong ligaments, increase the sacroiliac joints’ stability and makes dislocations very rare. The fossae lumbales laterales (“dimples of Venus“) correspond to the superficial topography of the sacroiliac joints.
Ligaments
- Anterior sacroiliac ligament
- Interosseous sacroiliac ligament
- Posterior sacroiliac ligament
- Sacrotuberous ligament
- Sacrospinous ligament
The anterior ligament is not much of a ligament at all and in most cases is just a slight thickening of the anterior joint capsule. The anterior ligament is thin and not as well defined as the posterior sacroiliac ligaments.
The posterior sacroiliac (SI) ligaments can be further divided into short (intrinsic) and long (extrinsic).[13] The dorsal interosseous ligaments are very strong ligaments. They are often stronger than bone, such that the pelvis may actually fracture before the ligament tears. The dorsal sacroiliac ligaments include both long and short ligaments. The long dorsal sacroiliac joint ligaments run in an oblique vertical direction while the short (interosseous) runs perpendicular from just behind the articular surfaces of the sacrum to the ilium and functions to keep the sacroiliac joint from distracting or opening. The extrinsic sacroiliac joint ligaments (the sacrotuberous and sacrospinous ligaments) limit the amount the sacrum flexes (or nutates).
The ligaments of the sacroiliac joint become loose during pregnancy due to the hormone relaxin; this loosening allows widening of the pelvic joints during the birthing process, especially the related symphysis pubis. The long SI ligaments may be palpated in thin persons for pain and compared from one side of the body to the other; however, the reliability and the validity of comparing ligaments for pain have currently not been shown. The interosseous ligaments are very short and run perpendicular from the iliac surface to the sacrum, they keep the articular surfaces from abducting or opening/distracting.
Physiology
Like most lower extremity joints, one of the SI joints’ function is shock absorption (depending on the amount of available motion at the sacroiliac joint) for the spine, along with the job of torque conversion allowing the transverse rotations that take place in the lower extremity to be transmitted up the spine. The SI joint, like all lower extremity joints, provides a “self-locking” mechanism (where the joint occupies or attains its most congruent position, also called the close pack position) that helps with stability during the push-off phase of walking.[14] The joint locks (or rather becomes close packed) on one side as weight is transferred from one leg to the other, and through the pelvis the body weight is transmitted from the sacrum to the hip bone.
The motions of the sacroiliac joint
- Anterior innominate tilt of both innominate bones on the sacrum (where the left and right move as a unit)
- Posterior innominate tilt of both innominate bones on the sacrum (where the left and right move together as a unit)
- Anterior innominate tilt of one innominate bone while the opposite innominate bone tilts posteriorly on the sacrum (antagonistic innominate tilt) which occurs during gait
- Sacral flexion (or nutation) Motions of the sacrum occur simultaneous with motion of the ilium so you must be careful in the description of these as isolated motions.
- Sacral extension (or counter-nutation).
The sacroiliac joints like all spinal joints (except the atlanto-axial) are bicondylar joints, meaning that movement of one side corresponds to a correlative movement of the other side.
Disorders
Pain is thought to be caused by sacroiliitis, an inflammation of one or both of the sacroiliac joint(s), which can be a common cause of unilateral low back pain. With sacroiliitis, the individual may experience pain in the low back, buttock or thigh, depending on the amount of inflammation. Common problems of the sacroiliac joint are often called sacroiliac joint dysfunction (also termed SI joint dysfunction; SIJD). The cause of sacroiliac joint dysfunction is likely a disruption of the correlative movements between the left and right sacroiliac joints (from either too much or too little movement creating an antagonistic position of the left and right innominate bones creating a pelvic obliquity, when they normally should appear symmetrical).
Another common disease associated with inflammation and pain of the sacroiliac joint(s) is Ankylosing spondylitis.
Symptoms and signs
The following are symptoms/signs that may be associated with an SI joint (SIJ) problem:
- Mechanical SIJ dysfunction usually causes a dull unilateral low back pain.[15]
- The pain is often a mild to moderate ache around the dimple or posterior superior iliac spine (PSIS) region.[16]
- The pain may become worse and sharp while doing activities such as standing up from a seated position or lifting the knee towards the chest during stair climbing.
- Pain is typically on one side or the other (unilateral PSIS pain), but the pain can occasionally be bilateral.
- When the pain of SIJ dysfunction is severe (which is infrequent), there can be referred pain into the hip, groin, and occasionally down the leg, but rarely does the pain radiate below the knee.
- Pain can be referred from the SIJ down into the buttock or back of the thigh, but rarely to the foot.
- Low back pain and stiffness, often unilateral, that often increases with prolonged sitting or prolonged walking.
- Pain may occur during sexual intercourse; however, this is not specific to just sacroiliac joint problems.
- Occasionally there may be referred pain into the lower limb, which can be mistaken for “true” sciatica from a herniated lumbar disc. This often can be differentiated from radicular (true nerve root pain) with a clinical test called the straight leg raising (SLR) test. This test, when negative, “rules out” > 90% of patients with true radicular or pain from a nerve root compression like a disc herniation/protrusion.[17]
Sacroiliac joint dysfunction is tested in many different ways, although the reliability of most individual tests has been shown to be low.[18] Using tests in combination will often improve their reliability.[19] Commonly used tests used to identify dysfunction include the Gillet Test (also called the Stork Test), the prone knee flexion test, the supine long sitting test, the standing flexion test, and the seated flexion test.[20] Another group of tests is called provocation tests; although these tests are not used to determine the type of sacroiliac joint dysfunction, they have been shown to be both reliable and valid for helping to determine the likely source of back pain.[21][22]Provocation tests include the FABER (Flexion, ABduction, External Rotation), thigh thrust, posterior shear, central posterior/anterior pressure on the sacrum, Gaenslen’s test, sacroiliac joint compression, and distracting (gapping) test. Like most sacroiliac joint tests, provocation tests do best when clustered together.[23][20] Description of the Gillet test:
- With the patient standing and the examiner sitting behind, the examiner’s left thumb is placed over the posterior most portion of the left posterior superior iliac spine (PSIS) and the right thumb overlying the midline of the sacrum at the same level.
- The examiner asks the patient to flex the left hip and knee as much as possible with a minimum of 90 degrees of the hip flexion (the key is that the hip has to flex beyond its maximal amount of motion so that the innominate bone can posteriorly tilt with hip flexion).
- A negative test finds the left thumb on the posterior superior iliac spine (PSIS) moving caudal (towards the tail) in relation to the right thumb on the sacrum.
- The thumb placements are reversed and the patient is asked to raise the right leg in similar fashion.
- A positive finding occurs when the thumb on the PSIS does not move at all or moves cranially (towards the head) in relation to the thumb on the sacrum.
- This test is designed to assess movement of the innominate bone posteriorly on the sacrum, thus if it does not move caudally the joint is not moving correctly in posterior tilt.
- The findings of this test are correlated with those of the standing flexion test or other sacroiliac joint tests.
- The Stork test is one test used to determine if the left or right SI joints may be restricted, since the reliability of this and many of the SIJ tests are poor the results of this test must agree or be consistent with other SIJ findings (e.g. signs and symptoms).
- If the patient has difficulty standing on one foot to perform the test, proprioceptive sensory motor balance deficit should be further evaluated.
Tests should be interpreted carefully since false positive and false negative test results are common, owing to their low reliability. A method that can reduce the findings of false positive and false negatives is to cluster the individual tests together. Finding 3 or 4 tests for a specific type of sacroiliac joint dysfunction, reduces the likelihood of false results. Adding a cluster of tests, along with the presence of absence of other sacroiliac joint symptoms and signs, can reduce the risk of spurious findings.[24] For the examiner to achieve success, however, the tests must agree with each other. There are many other tests available.[22] Passive mobility tests can be used to evaluate the hip, sacroiliac joint, and lumbar spine (again clinicians must be careful because of the low reliability of many of these tests). Some clinicians recommend the use of spring tests. These are performed with various positions, such as having the person lie prone, supine, sitting, side-lying, prone extension and prone flexion.
The most current research shows that palpation tests for diagnosis of sacroiliac joint dysfunction has been proven to not be a valid descriptor of sacroiliac joint position. (21) Also, it has been shown that a comprehensive McKenzie evaluation allows for excellent diagnostic accuracy in identifying patients with sacroiliac joint dysfunction as opposed to patients with lumbar diskogenic problems. (21)
Pregnancy
The hormonal changes of menstruation, pregnancy, and lactation can affect the integrity of the ligament support around the SIJ, which is why women often find the days leading up to their period are when the pain is at its worst. During pregnancy, female hormones are released that allow the connective tissues in the body to relax. The relaxation is necessary so that during delivery, the female pelvis can stretch enough to allow birth. This stretching results in changes to the SIJs, making them hypermobile—extra or overly mobile. Over a period of years, these changes can eventually lead to wear-and-tear arthritis. As would be expected, the more pregnancies a woman has, the higher her chances of SI joint problems. During the pregnancy, micro tears and small gas pockets can appear within the joint.
Muscle imbalance, trauma (e.g. falling on the buttock) and hormonal changes can all lead to SIJ dysfunction. Sacroiliac joint pain may be felt anteriorly, however care must be taken to differentiate this from hip joint pain.
Women are considered more likely to suffer from sacroiliac pain than men, mostly because of structural and hormonal differences between the sexes, but so far no credible evidence exists that confirms this notion. Female anatomy often allows one less sacral segment to lock with the pelvis, and this may increase instability.
See also
References
- ^ a b Solonen KA (1957). “The sacroiliac joint in the light of anatomical, roentgenological and clinical studies”. Acta Orthop Scand Suppl 27: 1–127.PMID 13478452.
- ^ Colachis SC, Worden RE, Bechtol CO, Strohm BR (September 1963). “Movement of the sacroiliac joint in the adult male: a preliminary report”. Arch Phys Med Rehabil44: 490–8. PMID 14050722.
- ^ Lavignolle B, Vital JM, Senegas J, et al. (1983). “An approach to the functional anatomy of the sacroiliac joints in vivo”. Anat Clin 5 (3): 169–76.doi:10.1007/BF01799002. PMID 6671062.
- ^ Butenas, Ann (February 2010). “Sacroiliac Joint Pain Information”. EmpowHER.
- ^ Smidt GL, McQuade K, Wei SH, Barakatt E (May 1995). “Sacroiliac kinematics for reciprocal straddle positions”. Spine 20 (9): 1047–54. doi:10.1097/00007632-199505000-00011.PMID 7631234.
- ^ Smidt GL, Wei SH, McQuade K, Barakatt E, Sun T, Stanford W (September 1997). “Sacroiliac motion for extreme hip positions. A fresh cadaver study”. Spine 22 (18): 2073–82. doi:10.1097/00007632-199709150-00003. PMID 9322317.
- ^ Sturesson B, Uden A, Vleeming A (February 2000). “A radiostereometric analysis of movements of the sacroiliac joints during the standing hip flexion test”. Spine 25 (3): 364–8. doi:10.1097/00007632-200002010-00018. PMID 10703111.
- ^ Weisl H (1955). “The articular surfaces of the sacro-iliac joint and their relation to movement”. Acta Anat. 22.
- ^ Wilder DG, Pope MH, Frymoyer JW (1980). “The functional topography of the sacroiliac joint”. Spine 5 (6): 575–9. doi:10.1097/00007632-198011000-00014. PMID 7466466.
- ^ Schunke G (1938). “The anatomy and development of the sacroiliac joint in man”.Anat Rec. 72 (3): 313–331. doi:10.1002/ar.1090720306.
- ^ Walker JM (1986). “Age-related differences in the human sacroiliac joint: a histological study; implications for therapy”. J Orthop Sports Phys Ther 7 (6): 325–34.PMID 18802258.
- ^ Alderink GJ (1991). “The sacroiliac joint: review of anatomy, mechanics, and function”. J Orthop Sports Phys Ther 13 (2): 71–84. PMID 18796854.
- ^ Weisl H (1954). “The ligaments of the sacroiliac joint examined with particular reference to their function”. Acta Anat (Basel) 20 (3): 201–13. doi:10.1159/000140900. PMID 13137770.
- ^ DonTigny RL (January 1985). “Function and pathomechanics of the sacroiliac joint. A review”(PDF). Phys Ther 65 (1): 35–44. PMID 3155567.
- ^ Cibulka MT, Delitto A & Erhard RE (1992). “Pain patterns in patients with and without sacroiliac joint dysfunction”. In Vleeming A, Mooney V, Snijders CJ & Dorman T (Eds.). Low Back Pain and it Relation to the Sacroiliac Joint. CA, 363–370: San Diego.
- ^ Fortin JD, Falco FJ (July 1997). “The Fortin finger test: an indicator of sacroiliac pain”. Am J. Orthop. 26 (7): 477–80. PMID 9247654.
- ^ Andersson GB, Deyo RA (December 1996). “History and physical examination in patients with herniated lumbar discs”. Spine 21 (24 Suppl): 10S–18S. PMID 9112321.
- ^ Freburger JK, Riddle DL (December 1999). “Measurement of sacroiliac joint dysfunction: a multicenter intertester reliability study”(PDF). Phys Ther 79 (12): 1134–41. PMID 10630282.
- ^ Karolina M Szadek et al., “Diagnostic validity of criteria for sacroiliac joint pain: a systematic review,” The Journal of Pain: Official Journal of the American Pain Society 10, no. 4 (April 2009): 354-368.
- ^ a b Cibulka MT, Delitto A, Koldehoff RM (September 1988). “Changes in innominate tilt after manipulation of the sacroiliac joint in patients with low back pain. An experimental study”(PDF).Phys Ther 68 (9): 1359–63. PMID 2971233.
- ^ Karolina M Szadek et al., “Diagnostic validity of criteria for sacroiliac joint pain: a systematic review,” The Journal of Pain: Official Journal of the American Pain Society 10, no. 4 (April 2009): 354-368.
- ^ a b Laslett M, Aprill CN, McDonald B (June 2006). “Provocation sacroiliac joint tests have validity in the diagnosis of sacroiliac joint pain”. Arch Phys Med Rehabil 87 (6): 874; author reply 874–5. doi:10.1016/j.apmr.2006.04.007. PMID 16731225.
- ^ Karolina M Szadek et al., “Diagnostic validity of criteria for sacroiliac joint pain: a systematic review,” The Journal of Pain: Official Journal of the American Pain Society 10, no. 4 (April 2009): 354-368.
- ^ Cibulka MT, Koldehoff R (February 1999). “Clinical usefulness of a cluster of sacroiliac joint tests in patients with and without low back pain”. J Orthop Sports Phys Ther 29 (2): 83–9; discussion 90–2. PMID 10322583.
21. Huijbregts P (2004). “Sacroiliac joint dysfunction: Evidence-based diagnosis”. Orthopaedic Division Review. p18–44. May/June.
From Wikipedia, the free encyclopedia http://en.wikipedia.org/wiki/Sacroiliac_joint
This work is licensed under a Creative Commons Attribution-ShareAlike 3.0 Unported License.